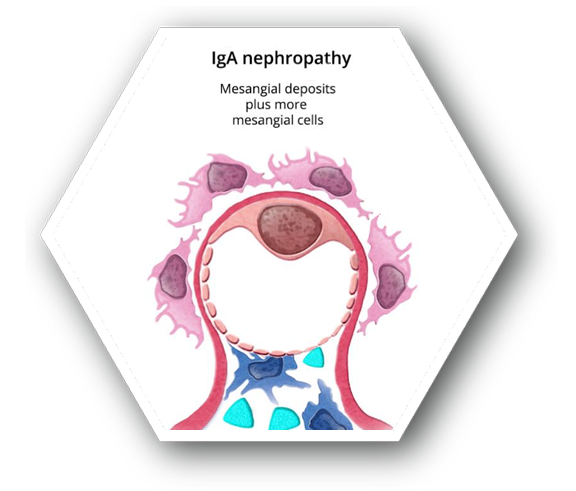
- Characterized by mesangial deposits of IgG-IgA1 immune complexes, which have been found to induce a inflammatory response and lead to a loss of kidney function6
-
Patients typically present with either macroscopic hematuria and proteinuria or persistent asymptomatic microscopic hematuria7
- Macroscopic hematuria typically follows a respiratory infection and presents with brown urine without clots
- Microscopic hematuria patients are typically asymptomatic and must be diagnosed with a urine test. Proteinuria may or may not be present
- Nephrotic syndrome is uncommon (only 5%)
- Older patients diagnosed late in life may have suffer from acute kidney injury or chronic kidney disease
- Incidence rate estimated to be about 2.5 patients/100,000 on average worldwide
- Higher male dominance
- Most common in Asia and southern Europe, followed by northern Europe and North America7
- Prognosis is typically good for most patients if proteinuria spilling is <0.2 g/24hr and normotensive
-
By age 20, ¼ of patients will suffer from ESRD
- An additional 20% of those patients will have progressive decline in estimated glomerular filtration rate
- Slow disease progression – highly dependent on hypertension and proteinuria levels6,7
ESRD: end-stage renal disease.
Recommendations are based on the KDIGO Clinical
Practice Guideline for Glomerulonephritis
-
Treatment aimed towards remission of proteinuria to slow progression of ESRD
- Prognosis goals: kidney survival and prevention of ESRD
- Options are based on degree and persistence of proteinuria and kidney function
-
Initial therapy upon diagnosis is dependent on proteinuria levels
- Non-nephrotic levels – supportive therapy of angiotensin-converting enzyme (ACE) inhibitors or angiotensin II receptor blockers (ARBs), followed by 6-month course of corticosteroids if proteinuria levels remain ≥1 g/day
- Crescentic IgAN with rapidly deteriorating kidney function – corticosteroids combined with immunosuppressive therapy
-
Non-steroidal immunosuppressive agents have some benefits in reducing nephrotic levels of proteinuria, but lack evidence to be used as a first line of defense
- Cyclophosphamide or azathioprine in combination with corticosteroids should only be used with rapidly deteriorating kidney function
-
As of 2012, the KDIGO guidelines list the following therapy as a potential treatment option, but there was insufficient data to make a recommendation for this agent:
- Mycophenolate mofetil (MMF)10
Alternative option not listed in 2012 KDIGO Guidelines
- The product is an FDA approved treatment option11
ESRD: end-stage renal disease.
Treatment Options
|
|
|---|---|
 Corticosteroids10 Corticosteroids10
|
 Cytotoxic Agents10 Cytotoxic Agents10
|
 Immunosuppressive Agents10 Immunosuppressive Agents10
|
 Acthar® Gel11* Acthar® Gel11*
|
*FDA approved, but not enough contemporaneous data for KDIGO to make a use recommendation